Virtual reality in surgical planning is revolutionizing the way surgeons prepare for complex procedures. Traditional methods often rely on 2D images and guesswork, which can lead to complications. In contrast, virtual reality offers a 3D immersive experience that enhances understanding of patient anatomy. Surgeons can practice their techniques in a simulated environment, boosting confidence and precision. This technology not only improves outcomes but also reduces surgery time. As healthcare evolves, integrating virtual reality into surgical planning becomes essential for better patient care. The future of surgery is here, making procedures safer and more efficient than ever before.
Key Takeaways
- Virtual reality (VR) can significantly enhance surgical planning by providing immersive simulations that help surgeons visualize complex procedures before they operate.
- One of the main benefits of using VR in surgery is improved decision-making, as it allows for better evaluation of patient-specific anatomy and potential complications.
- Surgeons should consider integrating VR tools into their medical workflows to streamline processes and improve overall efficiency.
- Enhancing spatial awareness through VR training can lead to better surgical outcomes, as it helps surgeons understand the 3D relationships of organs and tissues.
- Collaborative planning with virtual tools fosters teamwork among medical professionals, enabling them to share insights and strategies effectively.
- As the technology evolves, addressing challenges such as imaging uncertainty will be crucial for maximizing the benefits of VR in surgical planning.
Understanding VR in Surgical Planning
Immersive Simulations
VR technology creates immersive simulations for surgical planning. Surgeons can enter a virtual environment that replicates the actual operating room. This allows them to practice procedures before performing them on real patients. The simulation includes realistic movements and interactions. Surgeons can manipulate virtual tools and visualize their actions in 3D.
This level of immersion helps build confidence. It also reduces anxiety about complex surgeries. Surgeons can rehearse difficult steps multiple times. They can adjust their techniques based on the simulated feedback. By doing this, they enhance their skills without risk to patients.
Visualizing Anatomy
VR plays a crucial role in visualizing complex anatomical structures pre-surgery. Traditional imaging methods like X-rays or MRIs provide flat images. These images often lack depth and detail. VR transforms these images into 3D models, providing a clearer view of anatomy.
Surgeons can explore these models from all angles. They can zoom in on specific areas of interest. This helps them understand the relationship between different organs and tissues. For example, during brain surgery, surgeons can identify critical blood vessels and nerves. This detailed visualization leads to better surgical outcomes.
Integration with Medical Imaging
The integration of VR with existing medical imaging technologies enhances its effectiveness. Medical imaging devices like CT scans and MRIs provide vital data. VR systems use this data to create accurate 3D representations of patient anatomy.
Surgeons can import imaging data directly into the VR system. This seamless integration allows for real-time updates as new images become available. It ensures that the virtual model reflects the most current information about the patient’s condition.
Training programs now incorporate VR alongside traditional methods. New surgeons can learn by interacting with real-life scenarios in a safe environment. They gain valuable experience without putting patients at risk.
Benefits of VR in Surgery
- Enhanced Preparation: Surgeons prepare better when they practice in a virtual space.
- Reduced Errors: Familiarity with procedures lowers the chance of mistakes.
- Improved Communication: Teams can visualize cases together, leading to better collaboration.
- Patient Education: Patients can see their conditions in 3D, improving understanding.
Key Benefits of VR in Surgery
Risk Reduction
VR significantly reduces surgical risks. It provides detailed pre-operative insights into patient anatomy. Surgeons can explore 3D models of organs and tissues before the actual procedure. This visualization helps identify potential complications. For example, a surgeon can detect unusual blood vessel patterns that may pose risks during surgery. By understanding these details, they can plan better and avoid mistakes.
The use of VR also allows for rehearsing complex procedures. Surgeons can practice on virtual patients. This practice enhances their skills and confidence. Studies show that surgeons who use VR simulations perform better in real surgeries. They make fewer errors, leading to safer operations for patients.
Cost Savings
VR has notable cost-saving potential in surgical settings. Traditional surgical planning often requires extensive physical resources. These include models or cadavers for training and planning purposes. With VR, these needs decrease significantly. Surgeons can access virtual models anytime, anywhere.
Hospitals save money by reducing material costs and minimizing waste. Fewer complications lead to shorter hospital stays. Patients recover faster when surgeries are performed with precision. This efficiency translates into lower overall healthcare costs.
A study from the Journal of Medical Internet Research found that hospitals implementing VR technology saw a 30% reduction in costs related to surgical training and preparation.
Precision and Efficiency
VR tools enhance both precision and efficiency in surgery. Surgeons can visualize the surgical field in a detailed manner. They see exactly where to cut or avoid during the operation. This level of detail improves outcomes dramatically.
Moreover, VR aids in time management during surgeries. Surgeons spend less time figuring out the anatomy during the procedure itself. They have already mapped out their approach using VR before entering the operating room. This preparedness leads to quicker surgeries and less anesthesia time for patients.
For instance, orthopedic surgeons using VR have reported a 20% decrease in operation time due to better planning and execution.
Enhancing Decision-Making with VR
Evaluating Scenarios
Virtual reality (VR) plays a critical role in evaluating multiple surgical scenarios. Surgeons can visualize different approaches to a procedure. This technology allows them to explore various techniques without the risk associated with actual surgery. For instance, a surgeon can simulate a complex heart surgery from different angles. They can assess how each technique affects the patient’s anatomy.
This evaluation process helps surgeons make informed decisions. They can predict potential complications before entering the operating room. By analyzing these scenarios, they enhance their confidence and precision during surgery.
Improving Accuracy
VR also improves diagnostic accuracy significantly. Surgeons can use this technology to review 3D models of patient scans. Detailed images help in understanding the unique aspects of each case. With VR, they can identify critical structures that may not be evident in traditional imaging techniques.
For example, a neurosurgeon might use VR to visualize brain tumors in relation to vital blood vessels. This insight aids in planning the safest route for removal. Improved accuracy leads to better outcomes and reduces recovery times for patients.
Simulating Conditions
Simulating patient-specific conditions is another powerful feature of VR. Surgeons create tailored strategies based on individual patient data. They can input details like age, medical history, and specific health issues into the simulation.
Using this personalized approach ensures that each surgical plan addresses the patient’s unique needs. A joint replacement surgeon might simulate the exact joint structure of a patient. This allows for precise adjustments during the actual procedure.
The ability to customize surgical plans using VR leads to more effective treatments. It enhances both the surgeon’s skills and the overall patient experience.
Improving Spatial Awareness
3D Perspective
Virtual reality (VR) offers a unique three-dimensional view of anatomical structures. Surgeons can explore organs and tissues in detail. This technology allows them to visualize complex relationships that are hard to grasp in traditional 2D images.
For instance, during a surgical planning phase, a surgeon can manipulate a virtual model of the patient’s anatomy. They can rotate and zoom in on specific areas. This interactive experience enhances their understanding of spatial relationships. It helps them identify potential obstacles or complications before surgery even begins.
Hand-Eye Coordination
VR also plays a crucial role in improving hand-eye coordination. Surgeons use VR simulations to practice various procedures. These simulations mimic real-life scenarios, allowing them to develop skills without the risk associated with actual surgeries.
Through repeated practice in a safe environment, surgeons enhance their depth perception. They learn to judge distances accurately and coordinate their movements effectively. Studies show that practicing in VR leads to better performance during real surgeries. Surgeons who train with VR often report increased confidence in their abilities.
Navigating Complex Environments
Surgical environments can be intricate and challenging to navigate. VR provides tools that help surgeons prepare for these complexities. By simulating the operating room, surgeons can familiarize themselves with the layout and equipment placement.
This preparation reduces stress during actual procedures. It enables them to focus on the task at hand rather than being distracted by unfamiliar surroundings. For example, a neurosurgeon might use VR to rehearse an operation on a brain tumor. They can visualize critical structures like blood vessels and nerves beforehand.
Moreover, VR training can improve teamwork among surgical teams. Members can practice together in a virtual setting, enhancing communication and coordination skills. This collaboration leads to smoother operations and better patient outcomes.
Real-Life Applications
Many hospitals have started integrating VR into their surgical training programs. For example, the Cleveland Clinic has utilized VR for orthopedic surgery training since 2018. They reported significant improvements in trainee performance after using VR simulations.
Another example is the use of VR for laparoscopic surgery training at the University of California, San Francisco. Their studies indicate that residents who trained with VR performed better in real surgeries compared to those who did not.
In summary, VR technology is transforming how surgeons plan and execute procedures. By enhancing spatial awareness, improving hand-eye coordination, and aiding navigation in complex environments, it prepares surgeons for successful outcomes.
Integrating VR into Medical Workflows
Implementation Steps
Incorporating virtual reality (VR) into surgical protocols requires clear steps. First, hospitals must assess their current workflows. They need to identify areas where VR can improve spatial awareness and enhance planning. Next, they should select appropriate VR tools that fit their specific needs. This involves evaluating software and hardware options.
After selecting the right technology, hospitals must integrate it into their existing systems. Staff members will need to adapt their current practices to include VR. This may involve modifying surgical checklists or pre-operative assessments. Testing the new system is crucial before full implementation. Feedback from surgeons and staff helps refine the process.
Training Requirements
Training medical staff is essential for effective use of VR tools. Surgeons, nurses, and technicians must understand how to operate the technology. Initial training sessions should cover basic functionality and features of the VR system. Hands-on practice allows staff to gain confidence in using the equipment.
Ongoing education is equally important. Regular workshops keep staff updated on new features or improvements. Hospitals might also consider creating a mentorship program. Experienced users can guide less experienced colleagues through real-life scenarios.
IT System Integration
Seamless integration with hospital IT systems is vital for data management. Effective data handling ensures that patient information remains secure and accessible. Hospitals must ensure that the VR tools can communicate with electronic health records (EHR). This connection allows for easy retrieval of patient data during surgical planning.
Compatibility with existing software is necessary for smooth operation. IT teams should work closely with vendors to address any technical challenges. Regular updates and maintenance are also crucial to avoid disruptions in workflow.
Data analytics plays a significant role in improving surgical outcomes. By analyzing data collected from VR simulations, hospitals can identify trends and make informed decisions. This leads to better patient care and more efficient procedures.
Collaborative Planning with Virtual Tools
Real-Time Collaboration
Virtual reality (VR) allows surgical teams to collaborate in real-time. Surgeons can connect from different locations. This technology enables them to share insights and strategies instantly. They can visualize a patient’s anatomy in a 3D space together. This shared experience improves teamwork and decision-making.
In 2020, a study highlighted the effectiveness of VR in remote surgeries. Teams used VR headsets to plan complex procedures. They could manipulate 3D models of patients’ organs. This approach led to better-prepared surgical teams. It also reduced the chances of complications during surgery.
Enhanced Communication
VR enhances communication between surgeons and other healthcare professionals. Traditional methods often lead to misunderstandings. With VR, everyone involved can see the same visual data. Surgeons can explain their plans clearly using 3D models. Other team members, like nurses and anesthesiologists, gain valuable context.
For instance, during a procedure planning meeting, a surgeon might use VR to show the exact area they will operate on. This clarity helps all team members understand their roles better. It also fosters a collaborative spirit among professionals.
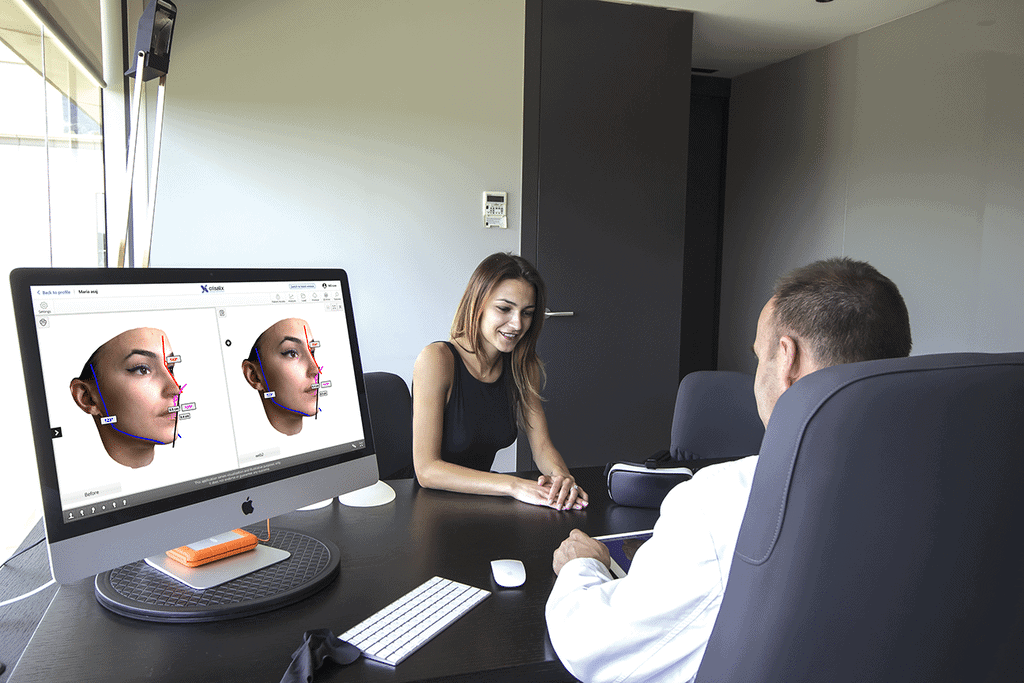
Patient Involvement
Virtual reality has potential for involving patients in their surgical planning process. Patients can explore 3D models of their own anatomy before surgery. This experience helps them understand the procedure better. It reduces anxiety by making the process more transparent.
In 2021, a hospital in California introduced VR for patient education. Patients used headsets to view their surgical plans. Many reported feeling more informed and confident about their procedures afterward. Engaging patients in this way promotes trust between them and their medical teams.
Benefits Overview
Using VR in surgical planning offers several benefits:
- Improved collaboration among surgical teams.
- Enhanced communication with clear visual aids.
- Patient involvement that boosts confidence.
These advantages contribute to better surgical outcomes and patient satisfaction.
Addressing Imaging Uncertainty
Enhancing Clarity
Virtual reality (VR) improves the clarity of medical images. Surgeons often face challenges when interpreting ambiguous images like CT scans or MRIs. VR technology allows them to visualize these images in a 3D format. This perspective helps surgeons see details that may be missed in traditional 2D views.
For example, a study conducted in 2020 showed that using VR increased the accuracy of tumor localization in lung surgeries. Surgeons could manipulate and rotate the images to gain a better understanding of the anatomy involved. This enhanced visualization leads to more informed decision-making.
Reducing Diagnostic Errors
VR provides additional perspectives that help reduce diagnostic errors. By immersing themselves in a virtual environment, surgeons can explore various angles of patient anatomy. This exploration aids in spotting abnormalities that might not be apparent from standard imaging alone.
A 2019 report highlighted how VR training simulations improved surgical outcomes by allowing residents to practice on virtual models before actual procedures. The ability to interact with these models helps identify potential issues early on, reducing the risk of errors during surgery.
Integrating Imaging Modalities
VR has the potential to integrate various imaging modalities for comprehensive analysis. It combines data from CT, MRI, and ultrasound into one cohesive view. This integration offers a complete picture of the patient’s condition.
For instance, a project launched in 2021 aimed to merge different imaging types into a single VR platform. This platform allowed surgeons to assess complex cases more thoroughly. They could analyze both soft tissue and bone structures simultaneously, leading to better surgical planning.
This multi-modal approach is crucial for intricate surgeries, such as those involving tumors near vital organs. By having all relevant information accessible in one environment, surgeons can devise more effective strategies.
Case Studies
Several case studies demonstrate the effectiveness of VR in addressing imaging uncertainty. In one case, a surgeon used VR to plan a complex spinal surgery. The surgeon analyzed multiple imaging sources and created a detailed virtual model of the spine. This preparation resulted in fewer complications during the operation.
Another study involved cardiac surgery planning using VR technology. Surgeons visualized heart structures from various angles, improving their understanding of blood flow dynamics. This insight led to more precise interventions and shorter recovery times for patients.
Challenges and Future Directions
Current Limitations
Current limitations hinder the widespread adoption of virtual reality in surgical planning. High costs remain a significant barrier for many hospitals and clinics. The expense of VR hardware and software can be prohibitive, especially for smaller facilities. The technology requires specialized training for surgeons and staff. Many healthcare professionals lack experience with VR systems, which can lead to resistance in using this innovative tool.
Another limitation involves the integration of VR with existing imaging technologies. While VR can enhance visualization, it often relies on accurate data from imaging techniques like MRI or CT scans. If the underlying images are unclear, the benefits of VR diminish. This situation creates uncertainty, which surgical teams must navigate during procedures.
Ongoing Research Needs
Ongoing research is essential to improve virtual reality applications in surgery. Developers need to focus on creating more user-friendly interfaces. A simpler design would encourage more surgeons to adopt VR technology. Research should also explore how to better integrate VR with other tools used in surgical planning.
Furthermore, studies must identify best practices for using VR in different types of surgeries. Each procedure has unique requirements that may affect how VR is applied. Understanding these nuances will help refine training programs for surgical teams.
Collaboration between tech companies and medical institutions can drive innovation in this field. Such partnerships can produce tailored solutions that meet specific surgical needs. They can also facilitate feedback from users, ensuring that new developments align with real-world demands.
Future Trends
Future trends suggest exciting possibilities for virtual reality in surgery. One significant advancement is the integration of artificial intelligence (AI). AI can analyze vast amounts of data quickly and accurately. This capability could enhance pre-surgical planning by predicting potential complications based on patient history.
AI could personalize VR experiences for individual patients. Surgeons might use tailored simulations based on a patient’s unique anatomy. This approach would improve preparation and increase confidence during actual procedures.
Another trend is the development of more immersive VR environments. These environments will allow surgeons to practice complex procedures before operating on patients. Enhanced realism will provide valuable hands-on experience without any risk to patients.
As technology evolves, virtual reality will likely become more accessible and affordable for surgical settings. Increased use of mobile devices may also contribute to this shift. Surgeons could utilize portable VR systems for quick consultations or training sessions.
Closing Thoughts
Virtual reality is a game-changer in surgical planning. It enhances decision-making, boosts spatial awareness, and integrates seamlessly into medical workflows. You can collaborate more effectively, address imaging uncertainties, and prepare for challenges ahead. The benefits are clear: improved outcomes and safer surgeries.
Embrace this technology to elevate your practice. Stay ahead of the curve and explore how VR can transform your surgical planning processes. Dive deeper into the potential of virtual reality and consider implementing it in your workflow. Your patients deserve the best, and VR might just be the key to achieving that.
Frequently Asked Questions
What is virtual reality in surgical planning?
Virtual reality (VR) in surgical planning involves creating 3D simulations of patient anatomy. Surgeons can visualize and rehearse procedures, enhancing precision and outcomes.
How does VR benefit surgeons?
VR offers immersive training, improved visualization, and better understanding of complex cases. This leads to more informed decisions and reduced surgical risks.
Can VR improve patient outcomes?
Yes, by allowing surgeons to practice and plan surgeries in a risk-free environment, VR can lead to fewer complications and faster recovery times for patients.
What role does spatial awareness play in surgery?
Spatial awareness is crucial for surgeons. VR enhances this skill by providing realistic representations of anatomy, helping surgeons navigate during procedures more effectively.
Is VR easy to integrate into existing medical workflows?
Integrating VR into medical workflows can be seamless with proper training and technology support. Many systems are designed to complement current practices without significant disruption.
How does VR facilitate collaborative planning?
VR enables multiple stakeholders—surgeons, radiologists, and other specialists—to interact within the same virtual environment. This fosters teamwork and ensures everyone is aligned on the surgical approach.
What challenges does VR face in surgical planning?
Challenges include high costs, technology adoption resistance, and the need for specialized training. However, ongoing advancements are addressing these issues for wider implementation.




