Breast Implant Rippling After Mastectomy: Prevention & Solutions
Understanding the Causes of Rippling
Thin Skin
Thin skin flaps and low body fat levels can make visible rippling of the breast implant more likely after a mastectomy, as breasts are reconstructed by a cosmetic surgeon aiming for optimal cosmetic results. These factors reduce the cushion over the implant in the breasts, making visible rippling more apparent and disrupting cosmetic results.
Patients with less natural tissue, especially in the pectoral coverage and inferolateral aspect, covering the implant often report seeing or feeling the outlines of their implants, impacting cosmetic results as noted by cosmetic surgeons. This is especially true in areas where movement is common, like the lower breast or side, where visible rippling, width, and figure solutions are crucial.
Implant Features
Implant size, width, and texture play crucial roles in rippling visibility, grade, figure, and solutions. Larger implants stretch the skin more, which can highlight ripples. Meanwhile, textured implants of a certain grade may grip the tissue better, reducing movement but not necessarily rippling or altering the figure.
Choosing the right grade of implant based on body type, desired outcome, and figure is vital. Surgeons often recommend breast implant options that balance aesthetics with the risk of visible ripples and grade.
Pocket Dynamics
The implant pocket’s size, location, and grade significantly affect rippling appearance. An improperly sized pocket can allow the implant to move excessively or sit unnaturally, exacerbating ripple visibility.
Submuscular placement (underneath muscle) generally offers better coverage and a higher grade for breast implant than subglandular placement (over muscle). It hides ripples more effectively in patients with thin skin or low body fat, especially when utilizing a high-grade breast implant.
Background Information on Implant Rippling
Commonality
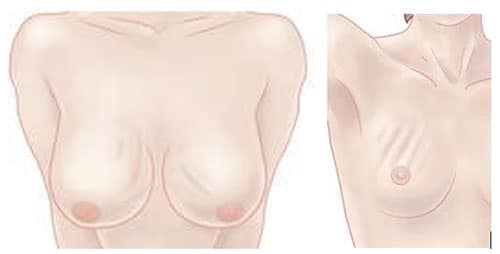
Implant rippling is a frequent concern for individuals who have undergone mastectomy and opted for breast implants of various grades. This condition manifests as visible waves or grade wrinkles on the surface of the implant, often noticeable under the skin.
Patients report breast implant issues not only as an aesthetic grade issue but also a source of discomfort. The prevalence of rippling varies, yet it significantly impacts those with thinner skin or less breast tissue post-mastectomy, depending on the grade.
Aesthetic Concerns
The appearance of rippling in breast implants can lead to dissatisfaction with surgical outcomes. For many, breast reconstruction is a step towards regaining normalcy and confidence after battling cancer. Visible implant imperfections can undermine this process, causing emotional distress.
Studies indicate that a significant portion of patients experience some degree of rippling post-surgery, particularly with breast implant procedures. The exact numbers vary, but the consensus underscores its commonality.
Psychological Impact
Beyond aesthetics, the psychological effect of implant rippling cannot be overstated. It may exacerbate feelings of self-consciousness or frustration in patients who have already endured much emotionally. Recognizing this impact is crucial in addressing patient concerns effectively.
Techniques for Correcting Implant Rippling
Surgical Options
Surgical interventions offer a direct approach to address implant rippling. One common method is the replacement of the implant with one of a different type or texture. This can significantly reduce the visibility of rippling, especially when switching from saline to silicone implants, which tend to have a more natural feel and less propensity for rippling.
Another surgical technique involves adjusting the implant pocket, either by repositioning the implant under the muscle (for those initially placed over it) or correcting the pocket size to better accommodate the implant. These adjustments can help in distributing pressure more evenly around the implant, minimizing rippling effects.
Non-Surgical Options
For those seeking less invasive methods, non-surgical options are available. Fat grafting stands out as a popular choice. It involves harvesting fat from another part of the body and injecting it around the implant area. This extra layer of fat can mask rippling by providing additional padding and improving skin quality over the implant.
However, fat grafting requires sufficient donor fat and may necessitate multiple sessions to achieve desired results, making it less suitable for everyone.
Customized Plans
The key to effectively correcting implant rippling lies in tailoring the treatment plan to each patient’s unique anatomy and needs. Factors such as skin thickness, body composition, and lifestyle should influence the choice between surgical and non-surgical options.
Implant exchange might be ideal for some, whereas others could benefit more from fat grafting or pocket adjustments. Consulting with a skilled surgeon who understands these nuances ensures that patients receive the most appropriate intervention for their specific situation.
Utilizing Allograft Dermis for Correction
Dermis Function
Allograft dermis acts as a natural barrier. It helps in hiding the rippling of breast implants post-mastectomy. This layer, when placed between the implant and the skin, offers extra padding. This reduces the visibility of wrinkles or ripples.
The dermis integrates with the patient’s own tissue over time. It strengthens the area around the implant. This process minimizes the chances of rippling reoccurring.
Selection Process
Choosing the right allograft dermis is crucial. Surgeons evaluate several factors before making a decision. These include the thickness of the dermis and its compatibility with the patient’s body.
Preparation involves sterilization and testing for diseases. Only then is it deemed safe for implantation alongside breast implants.
Success Rates
Studies show high success rates with allograft dermis in correcting rippling. Most patients report significant improvements in appearance and feel more confident.
Patient satisfaction scores are consistently high among those who undergo this procedure. They appreciate the natural look and feel that allograft dermis provides.
Preoperative Planning and Patient Selection
Patient Criteria
Selecting the right patients for allograft dermis insertion is crucial. It begins with understanding their needs and the specific challenges they face post-mastectomy. Not all patients will experience severe rippling, but for those who do, especially in the upper pole of the breast, this treatment can be a game-changer.
Patients with a noticeable absence of tissue or those who have experienced significant weight changes may benefit most. The width and appearance of the breast after mastectomy are also key factors. These criteria help in tailoring a personalized approach that addresses each patient’s unique situation.
Evaluation Process
The evaluation process is thorough. It involves assessing the extent of rippling and deciding on the best corrective approach. This step is critical to ensure that the chosen method aligns with the patient’s expectations and desired outcome.
Doctors use various techniques to measure the severity of rippling and determine if allograft dermis insertion is suitable. They consider consecutive patients’ histories, examining previous treatments and their outcomes. This comprehensive review helps predict potential success rates for individual cases.
Managing Expectations
Managing expectations is perhaps the most important aspect of preoperative planning. Patients need to understand what the procedure can realistically achieve. Clear communication about possible outcomes, including improvements in appearance and any limitations, sets a solid foundation for patient satisfaction.
Doctors should discuss all options available, emphasizing that while allograft dermis can significantly reduce rippling, it may not completely eliminate it. This honesty helps build trust and ensures patients make informed choices about their treatment.
Detailed Surgical Correction Technique
Surgical Steps
Following careful preoperative planning, the correction of implant rippling begins. The cosmetic surgeon first addresses the capsular contracture by loosening or removing the tight capsule. This step is crucial for creating a more natural look and feel.
The surgeon then focuses on the inferolateral aspect of the breast, where rippling is most common. By tightening this area and ensuring proper pectoral coverage, they can significantly reduce the visibility of rippling.
Allograft Types
For enhancing structural support, allograft dermis is used. There are several types of allografts available, each with its own set of benefits. The choice depends on the patient’s specific needs and the surgeon’s preference.
The use of acellular dermal matrix (ADM) has become popular due to its ability to integrate with the patient’s tissue, providing additional strength to the weakened area. Surgeons may also opt for other materials based on their texture and integration capabilities.
Postoperative Care
Post-surgery, meticulous care is essential for healing and minimizing complications. Patients must follow a strict regimen that includes wound care, limited physical activity, and regular follow-up appointments.
Monitoring involves checking for signs of infection, ensuring proper position of the implant, and assessing the health of the overlying skin. Adherence to these guidelines helps achieve optimal results and satisfaction.
Discussing Effectiveness and Potential Complications
Case Studies
Recent data shows the effectiveness of using allograft dermis to reduce breast implant rippling after mastectomy. A series of case studies highlight significant improvements in cosmetic results. Patients reported higher satisfaction rates due to minimized disruption in the breast area.
The use of specific materials plays a crucial role. It increases the volume around the implant, which effectively masks any potential rippling. This solution has become a preferred method for many.
Complication Management
Despite the high success rate, some patients may experience complications. The main risks include infection and an increase in recovery time. However, these are manageable with proper care and follow-up.
Weight loss or gain can also affect the outcome. It may lead to changes in breast volume, which could cause rippling to reappear over time. Thus, maintaining a stable weight is advised for long-term satisfaction.
Long-Term Outcomes
Patients undergoing correction for implant rippling often report long-term aesthetic improvements. The added volume from allograft dermis not only addresses immediate concerns but also enhances the overall appearance of breasts post-mastectomy.
Factors such as material choice and surgical technique play vital roles in these outcomes. Patients appreciate the natural feel and look, citing it as a major reason for their satisfaction.
Final Remarks
Breast implant rippling after a mastectomy can be unsettling, but understanding the causes and exploring corrective techniques is your first step towards resolution. From utilizing allograft dermis to detailed surgical correction strategies, you’ve got options. Remember, preoperative planning and selecting the right patient are crucial to enhancing effectiveness while minimizing potential complications. Your journey to reclaiming your body’s appearance post-mastectomy is personal and unique. By staying informed and consulting with experienced professionals, you’re empowered to make choices that align with your goals and well-being.
Don’t let the fear of implant rippling hold you back. Reach out to a specialist today, discuss your concerns, and explore the best corrective measures for you. Your confidence and comfort matter. Take that step towards a more assured tomorrow.
Frequently Asked Questions
What causes rippling in breast implants after mastectomy?
Rippling occurs due to thinning breast tissue or insufficient coverage over the implant, making the edges or texture of the implant visible through the skin.
How can rippling in breast implants be corrected?
Techniques include adjusting the implant position, switching to a different type of implant, or using tissue matrices like allograft dermis to provide better coverage and support.
Is utilizing allograft dermis effective for correcting implant rippling?
Yes, utilizing allograft dermis has been shown to effectively provide additional coverage and support, reducing the visibility of rippling in breast implants.
What should be considered during preoperative planning to prevent implant rippling?
Considerations include assessing patient’s tissue characteristics, choosing the right type and size of implant, and discussing expectations to select the best surgical approach for each individual.
Can you describe the detailed surgical correction technique for implant rippling?
The technique involves careful adjustment or replacement of the existing implant, possibly combined with tissue matrix placement for enhanced support and coverage. Each procedure is tailored to the patient’s specific needs.
How effective is surgical correction for breast implant rippling?
Surgical correction has a high success rate in reducing or eliminating rippling, significantly improving aesthetic outcomes and patient satisfaction when performed by experienced surgeons.
What are potential complications of correcting breast implant rippling?
While generally safe, potential complications can include infection, bleeding, changes in nipple sensation, or need for further surgery. Choosing a skilled surgeon minimizes these risks.






